Preparing for DVT Awareness Month
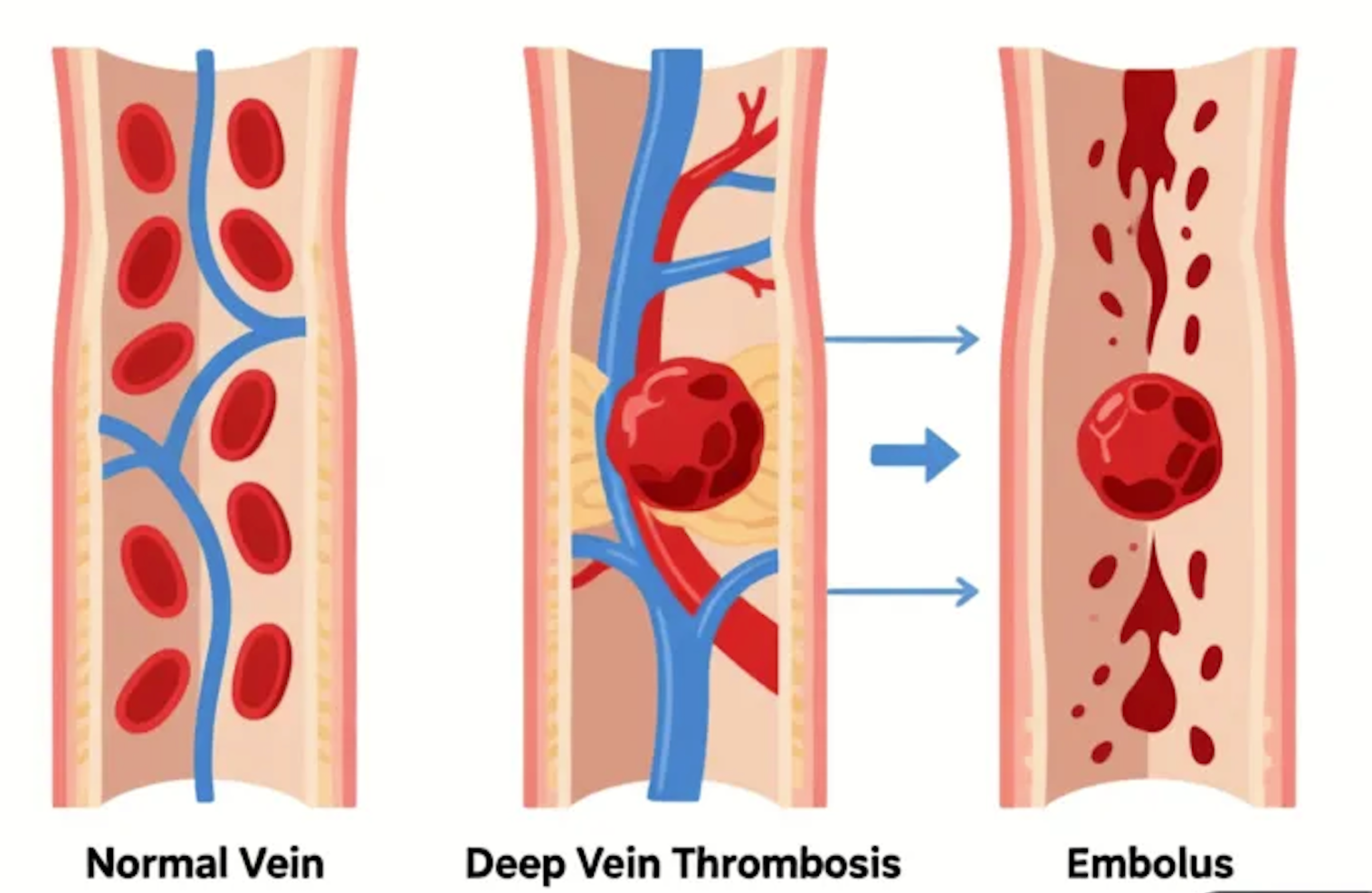
March marks Deep Vein Thrombosis (DVT) Awareness Month, an important time to educate ourselves about this serious but often preventable condition. DVT occurs when a blood clot forms in a deep vein, usually in the legs. While the condition itself is concerning, the real danger lies in potential complications, particularly pulmonary embolism, which can be life-threatening if a clot breaks free and travels to the lungs.
Understanding your personal risk factors and recognizing warning signs can literally save your life. DVT Awareness Month provides an opportunity to assess your risk, learn prevention strategies, and take proactive steps to protect your vascular health.
Understanding Deep Vein Thrombosis
Blood clots form when blood flow slows or stagnates, allowing clotting factors in the blood to accumulate rather than being dispersed by normal circulation. Deep veins, particularly those in the legs, are most susceptible because they must work against gravity to return blood to the heart.
DVT develops through three primary mechanisms: blood flow stasis, blood vessel damage, and hypercoagulability. When one or more of these factors are present, the risk of clot formation increases significantly. The condition can affect anyone, but certain circumstances dramatically elevate risk.
The potential consequences make DVT a medical emergency requiring prompt attention. A clot in the leg vein can cause pain, swelling, and long-term damage to the vein valves. More seriously, if a portion of the clot breaks away, it can travel through the bloodstream to the lungs, blocking blood flow and causing a pulmonary embolism. This complication can cause sudden difficulty breathing, chest pain, rapid heart rate, and in severe cases, can be fatal.
Major Risk Factors for DVT
Certain situations and characteristics significantly increase your likelihood of developing a blood clot. Recent surgery or major injury top the list of risk factors. Surgical procedures, particularly those involving the legs, hips, pelvis, or abdomen, can damage blood vessels and trigger the clotting cascade. The period of immobility during and after surgery compounds this risk. Even minor surgeries carry some increased risk, especially if they require anesthesia and bed rest.
Prolonged immobility from any cause creates conditions ripe for clot formation. Long-distance travel, particularly flights lasting more than four hours, keeps you seated with restricted movement. Hospital stays or bed rest due to illness prevent the muscle pump action that normally aids blood return. Even extended periods of sitting at work without movement breaks can contribute to sluggish circulation. Understanding how to prevent blood clots when traveling is crucial for frequent flyers and road-trippers.
Pregnancy and the postpartum period bring multiple DVT risks. The growing uterus puts pressure on pelvic veins, slowing blood flow from the legs. Hormonal changes during pregnancy make blood more prone to clotting as a protective mechanism against excessive bleeding during delivery. The risk remains elevated for several weeks after giving birth. Managing vein health during pregnancy requires awareness and preventive measures.
Hormonal medications, including birth control pills, hormone replacement therapy, and fertility treatments, can increase clotting tendency. The estrogen component in these medications affects clotting factors in the blood. Women who take hormonal medications and have additional risk factors face compounded risk and should discuss this with their healthcare providers.
Medical Conditions That Increase Risk
Certain health conditions predispose individuals to blood clots.
Cancer and Its Treatments
Cancer and its treatments can increase clotting risk through multiple mechanisms. Tumors can produce substances that activate the clotting system, and chemotherapy can damage blood vessels. Some cancers are more strongly associated with clots than others, particularly pancreatic, lung, and brain cancers.
Heart Conditions
Heart conditions, including heart failure and heart attac,k affect circulation throughout the body. When the heart doesn't pump efficiently, blood flow slows, creating conditions favorable for clot formation. Inflammatory diseases such as inflammatory bowel disease and certain autoimmune conditions increase inflammation throughout the body, including in blood vessel walls, which can trigger clotting.
Clotting Disorders
Inherited clotting disorders affect how blood coagulates. Conditions like Factor V Leiden mutation or prothrombin gene mutation are genetic abnormalities that make blood more likely to clot. Many people don't know they carry these conditions until they experience a clotting event or undergo genetic testing after a family member's diagnosis.
Previous DVT
Previous DVT or pulmonary embolism dramatically increases the risk of recurrence. Once you've had one clot, your veins may have sustained damage that makes future clots more likely. Additionally, whatever factors caused the first clot may still be present unless addressed.
Lifestyle and Demographic Factors
Beyond medical conditions, various lifestyle factors influence DVT risk. Obesity places additional pressure on leg veins and affects blood flow patterns. Excess weight is also associated with inflammation and metabolic changes that can increase clotting tendency. Even modest weight loss can reduce risk significantly.
Smoking damages blood vessels and affects blood clotting factors. It promotes inflammation and makes blood more likely to form clots. The risk increases with the number of cigarettes smoked and years of smoking, but fortunately, the risk decreases after quitting.
Age is an unavoidable risk factor. People over 60 face a higher risk as veins naturally lose elasticity and valve function declines with age. However, DVT can occur at any age, especially when other risk factors are present.
A family history of blood clots suggests possible genetic factors that increase risk. If close relatives have had DVT or pulmonary embolism, especially at young ages or without obvious triggers, genetic clotting disorders may run in your family.
Recognizing DVT Symptoms
Early recognition of DVT symptoms allows for prompt treatment and can prevent serious complications. Classic symptoms typically affect one leg and include swelling, which may develop suddenly and can range from mild to dramatic. Leg swelling that appears quickly or affects only one side requires immediate evaluation.
Pain or tenderness often begins in the calf and may feel like a cramp or charley horse. The pain typically worsens when walking or standing and may improve with rest. Skin color changes appear as the affected leg may look red, pale, or have a bluish tint. Warmth is another telltale sign, as the leg may feel noticeably warmer to the touch compared to the other leg.
However, not all DVTs cause obvious symptoms. Some people have "silent" clots that aren't detected until they cause complications. This makes awareness of risk factors and preventive measures even more critical.
Pulmonary Embolism: A Life-Threatening Emergency
When a clot travels to the lungs, symptoms require immediate emergency care. Sudden difficulty breathing or shortness of breath that comes on quickly is a red flag. Chest pain that worsens with deep breathing or coughing suggests pulmonary involvement. Rapid or irregular heartbeat, coughing up blood (even small amounts), feeling lightheaded or fainting, and anxiety or a sense of impending doom all require immediate medical attention.
If you experience any of these symptoms, especially if you have known risk factors for DVT, call emergency services immediately. Time is critical in treating pulmonary embolism, and early intervention can be life-saving.
Prevention Strategies for High-Risk Individuals
If you know you're at elevated risk for DVT, several proactive measures can significantly reduce your chances of developing a clot.
1. Stay Mobile
Stay mobile as much as possible. When facing situations that require immobility, such as surgery or long travel, talk to your doctor about prevention strategies. Compression stockings provide external pressure that helps blood flow upward. Wear them during long flights, after surgery, or whenever advised by your healthcare provider.
2. Blood Thinners
Blood-thinning medications may be prescribed if you're at particularly high risk. These anticoagulants prevent clots from forming but must be taken exactly as directed. Never stop or start these medications without medical guidance. For people undergoing surgery, prophylactic blood thinners are often given to prevent clots during the high-risk perioperative period.
3. Regular Exercise
Staying active and maintaining movement is one of the most effective prevention strategies. Regular exercise strengthens your cardiovascular system and keeps blood flowing smoothly. When travel or work requires extended sitting, perform simple exercises like ankle pumps, calf raises, and leg lifts every hour.
4. Hydration
Hydration helps maintain proper blood viscosity. Dehydration thickens blood, making it more prone to clotting. Aim for adequate water intake throughout the day, especially during situations that increase risk, like air travel or illness.
The Importance of Awareness
DVT Awareness Month serves as a reminder that blood clots are both serious and preventable. Education empowers people to recognize their risks, take appropriate preventive measures, and seek help quickly when symptoms develop.
Understanding DVT doesn't require medical training, but it does require attention to your body and awareness of circumstances that increase risk. Simple lifestyle modifications can dramatically reduce your chances of experiencing this dangerous condition.
Share information about DVT with family members, particularly those who may be at risk due to age, medical conditions, or upcoming surgeries. Awareness spreads through conversation, and the knowledge you share might save someone's life.
Moving Forward With Confidence
Understanding DVT risk factors and prevention strategies provides peace of mind and practical tools for protecting your health. While we can't eliminate all risk, we can dramatically reduce it through awareness and appropriate action.
This March, commit to prioritizing your vascular health. Whether that means adding daily walks to your routine, staying hydrated, wearing compression stockings during travel, or seeking medical evaluation for concerning symptoms, every positive action supports your circulatory system.
DVT is serious but largely preventable. Armed with knowledge and equipped with prevention strategies, you can significantly reduce your risk and respond appropriately if symptoms develop. That's the true power of awareness.
Elmore Medical Vein & Laser Treatment Center is the premier vein specialty medical practice in the Central Valley. Dr. Mario H. Gonzalez and his staff offer years of experience and medical expertise that you won’t find anywhere else. Contact us to set up a consultation appointment.